Managing Type 1 and Type 2 for a Healthier Life
Diabetes is one of the most prevalent chronic conditions in the UK, affecting millions of people each year. With the increasing number of people diagnosed with both Type 1 and Type 2 diabetes, it’s crucial to have a clear understanding of the condition, how it affects your body, and how to manage it effectively. Whether you are living with diabetes or concerned that you may be at risk, knowledge is power. Early intervention, healthy lifestyle choices, and ongoing medical support can help you control the condition and maintain a fulfilling life.
What is Diabetes?
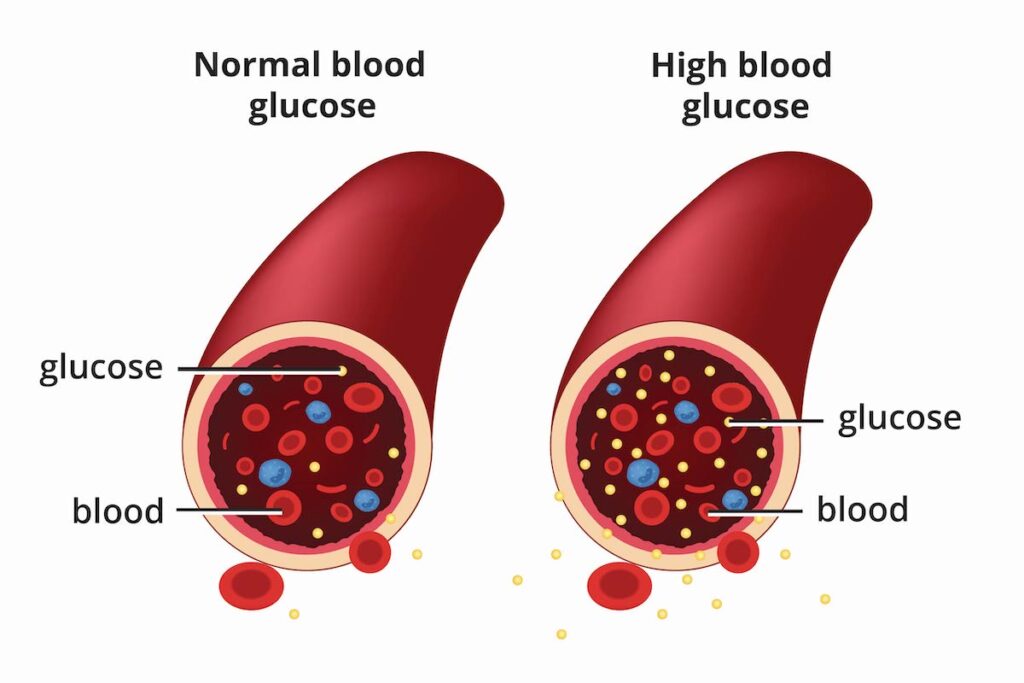
Diabetes is a metabolic disorder that affects how your body processes blood sugar (glucose). The body needs glucose for energy, but to use it effectively, it requires insulin, a hormone produced by the pancreas. Insulin helps cells absorb glucose from the bloodstream, but in diabetes, this process is disrupted.
There are two main types of diabetes: Type 1 and Type 2. Both affect blood sugar control but differ in their causes, symptoms, and management strategies.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas, known as beta cells. As a result, the pancreas can no longer produce insulin, and people with Type 1 diabetes must take insulin externally, either through injections or an insulin pump, to regulate their blood sugar levels.
Type 1 diabetes typically develops in childhood or early adulthood, although it can occur at any age. The exact cause remains unclear, but it’s believed that genetic factors, as well as environmental triggers like viral infections, may play a role in its development.
Symptoms of Type 1 Diabetes:
Rapid weight loss despite an increased appetite
Excessive thirst (polydipsia)
Frequent urination (polyuria)
Fatigue and lethargy
Blurred vision
Nausea or vomiting (in more severe cases)
Managing Type 1 Diabetes:
Insulin Therapy: Individuals with Type 1 diabetes require lifelong insulin therapy. This can be in the form of injections or via an insulin pump, which delivers a continuous supply of insulin. There are different types of insulin, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin. A healthcare professional will tailor the type and dosage based on individual needs.
Blood Sugar Monitoring: Monitoring blood glucose levels regularly is essential. This allows individuals to adjust their insulin dosage and take action to avoid hypoglycaemia (low blood sugar) or hyperglycaemia (high blood sugar). Continuous glucose monitors (CGMs) are available for more constant monitoring.
Healthy Diet and Carbohydrate Counting: A balanced diet is key to managing Type 1 diabetes. Carbohydrates have the most significant impact on blood sugar levels, so it’s essential to count carbs and make informed food choices. A registered dietitian can help create a meal plan tailored to individual needs.
Physical Activity: Exercise helps lower blood sugar levels and improves insulin sensitivity. However, it is important to monitor blood sugar before, during, and after exercise to avoid hypoglycaemia.
Emotional Support: Coping with Type 1 diabetes can be emotionally challenging. Support groups, counselling, and diabetes education can help individuals manage the emotional side of living with a chronic condition.
Type 2 Diabetes
Type 2 diabetes is the more common form of the condition, accounting for approximately 90% of all diabetes cases in the UK. Unlike Type 1, Type 2 diabetes develops when the body either becomes resistant to insulin or doesn’t produce enough insulin to maintain normal blood sugar levels. Over time, the body’s inability to manage blood sugar leads to elevated glucose levels, which can cause long-term damage to organs and tissues.
Type 2 diabetes is most common in adults over the age of 40, though increasing numbers of younger people are being diagnosed due to rising levels of obesity, poor diet, and lack of physical activity. In some cases, it may be possible to prevent or delay the onset of Type 2 diabetes by making healthy lifestyle changes.
Symptoms of Type 2 Diabetes:
Increased thirst and urination
Feeling more tired than usual
Unexplained weight loss
Slow-healing cuts or sores
Blurred vision
Numbness or tingling in the hands or feet
Dark patches of skin, typically in the armpits or neck (known as acanthosis nigricans)
Managing Type 2 Diabetes:
Lifestyle Changes: One of the most effective ways to manage Type 2 diabetes is through lifestyle modifications. Losing weight, eating a healthy diet, and increasing physical activity can significantly improve insulin sensitivity and help lower blood sugar levels.
Dietary Adjustments: A healthy diet that is rich in fibre, whole grains, lean proteins, and healthy fats can help manage blood sugar levels. It’s important to limit sugary foods, refined carbohydrates, and processed snacks. Consulting with a dietitian can help ensure you’re making the right food choices for your condition.
Physical Activity: Regular exercise is critical in managing Type 2 diabetes. Physical activity helps the body utilise insulin more effectively and lowers blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week, such as walking, swimming, or cycling.
Medication: If lifestyle changes alone are not enough to control blood sugar levels, medications may be prescribed. Oral medications, such as metformin, can help the body utilise insulin better, while others may increase insulin production or slow the absorption of sugar from food. In some cases, insulin therapy may be required.
Blood Sugar Monitoring: Regularly checking blood sugar levels allows individuals to track their progress and make adjustments to their diet, activity level, or medications. The goal is to keep blood sugar levels within a target range set by your healthcare provider.
Managing Complications: Managing Type 2 diabetes also involves regular checks for potential complications, such as kidney disease, eye problems, and nerve damage. Early intervention can help reduce the risk of complications.
Spotting the Signs: Are You at Risk?
For people with Type 1 diabetes, symptoms typically develop quickly and may be severe. However, Type 2 diabetes can develop gradually, and many people may not experience noticeable symptoms until the condition has progressed. In some cases, Type 2 diabetes may go undiagnosed for years, leading to complications such as heart disease, stroke, and nerve damage.
Risk Factors for Type 2 Diabetes:
Being overweight or obese: Excess fat, especially around the abdomen, increases the risk of insulin resistance.
Physical inactivity: A sedentary lifestyle contributes to weight gain and poor insulin sensitivity.
Age: People over 40 are at higher risk for Type 2 diabetes, although the condition is becoming more common in younger individuals due to lifestyle factors.
Family history: Having a close family member, such as a parent or sibling, with diabetes increases the risk.
Ethnicity: People of South Asian, African, or Caribbean descent are at a higher risk of developing Type 2 diabetes.
High blood pressure or high cholesterol: These conditions often occur alongside Type 2 diabetes and increase the risk of complications.
What to Do If You Think You Might Have Diabetes
If you suspect you have diabetes or are at risk, it’s important to take action as soon as possible. Early diagnosis and intervention can prevent or delay complications and help you live a long, healthy life.
Book an Appointment with Your GP: If you notice symptoms or are concerned about your risk, your GP can arrange a simple blood test to check your blood sugar levels. The sooner you catch the condition, the easier it is to manage.
Pre-Diabetes: If your blood sugar levels are higher than normal but not yet in the diabetic range, you may have pre-diabetes. This is a critical stage where lifestyle changes can prevent the progression to Type 2 diabetes.
Regular Check-Ups: Once diagnosed, regular check-ups with your GP, diabetic nurse, or dietitian are essential for monitoring and adjusting your treatment plan.
Prevention: Taking Control of Your Health
While Type 1 diabetes cannot be prevented, Type 2 diabetes is largely preventable with the right lifestyle choices. Maintaining a healthy weight, staying physically active, and eating a nutritious, balanced diet can reduce your risk significantly.
Healthy Eating: Embrace a diet rich in whole foods like fruits, vegetables, lean proteins, and whole grains, and avoid excessive consumption of processed foods, sugar, and refined carbohydrates.
Exercise Regularly: Engage in at least 30 minutes of moderate-intensity exercise most days of the week, such as walking, cycling, or swimming.
Weight Management: Losing even a small amount of weight can help improve insulin sensitivity and lower the risk of Type 2 diabetes.
Taking these simple yet powerful steps can significantly reduce your risk of developing Type 2 diabetes and help you manage your health effectively.
Diabetes is a complex condition, but with the right understanding and approach, it’s possible to manage both Type 1 and Type 2 diabetes successfully. Whether you’ve been diagnosed or are concerned about your risk, making informed choices about your diet, exercise, and healthcare can help you lead a healthy life. Speak to your GP or diabetes specialist for personalised advice and support, and remember, taking control of your health today can have lasting benefits for your future.
This article aims to provide you with a comprehensive understanding of diabetes and the steps you can take to manage or prevent the condition. The key to diabetes management is staying informed, making proactive lifestyle changes, and seeking support from healthcare professionals